Release time :2025-01-10
Source:support@yingchitech.com
Scan:705
Autism spectrum disorder (ASD) is a complex neurodevelopmental syndrome behaviorally defined by persistent deficits in social communication and interaction, along with stereotyped behaviors, interests, and activities. Transcranial magnetic stimulation (TMS) offers a potential intervention for ASD by mitigating its core and associated symptoms. While reviews on TMS treatment for ASD have been published, there has been a lack of systematic reviews since 2018 addressing research characteristics, specific stimulation parameters, localization techniques, stimulation targets, behavioral outcomes, and changes in neuroimaging biomarkers. To address this gap, this review systematically searched the literature published since 2018 on PubMed, Web of Science, and Science Direct.
Currently, ASD affects approximately 1% of the global population, predominantly males, with over 70% of cases presenting comorbidities. Treatment for ASD typically involves behavioral and pharmacological approaches. Behavioral training is the most effective intervention; however, it is both expensive and time-consuming. On the other hand, since no biomedical treatments targeting the core symptoms of ASD have been identified, the efficacy of pharmacological treatment is limited to addressing ASD-associated symptoms. It does not address the underlying core symptoms and often comes with significant side effects. Given the abnormal synaptic plasticity and excitatory/inhibitory ratio in ASD, combined with the ability of transcranial magnetic stimulation (TMS) to modulate cortical excitability and plasticity, the potential of TMS in ASD research has begun to be explored in laboratories worldwide.
Study Types: The review included studies published in English between January 1, 2018, and June 5, 2023. These comprised randomized controlled trials, controlled trials, parallel trials, single-blind trials, and double-blind trials.
Participant Types: Subjects were patients of any age or gender with a preliminary clinical diagnosis of ASD based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), DSM-4, the Autism Spectrum Quotient (AQ), the Autism Diagnostic Observation Schedule-2 (ADOS-2), or clinical diagnosis by a physician.
Intervention Type: Transcranial Magnetic Stimulation (TMS) used either as a standalone treatment or in combination with other interventions.
Outcome Measures:
Data Sources: Eligible studies from PubMed, Web of Science, and Science Direct published between January 1, 2018, and June 5, 2023.
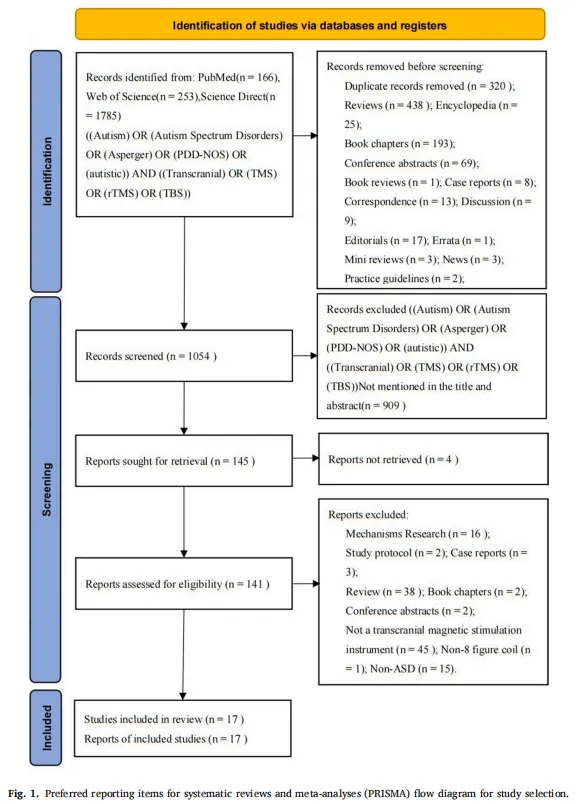
The systematic review ultimately included 17 studies, consisting of 7 randomized controlled trials and 10 open-label studies. The age of participants ranged from 2 to 30 years. However, a significant number of retrospective studies demonstrated a moderate to high risk of bias, primarily due to the lack of blinding of participants and assessors during treatment allocation.
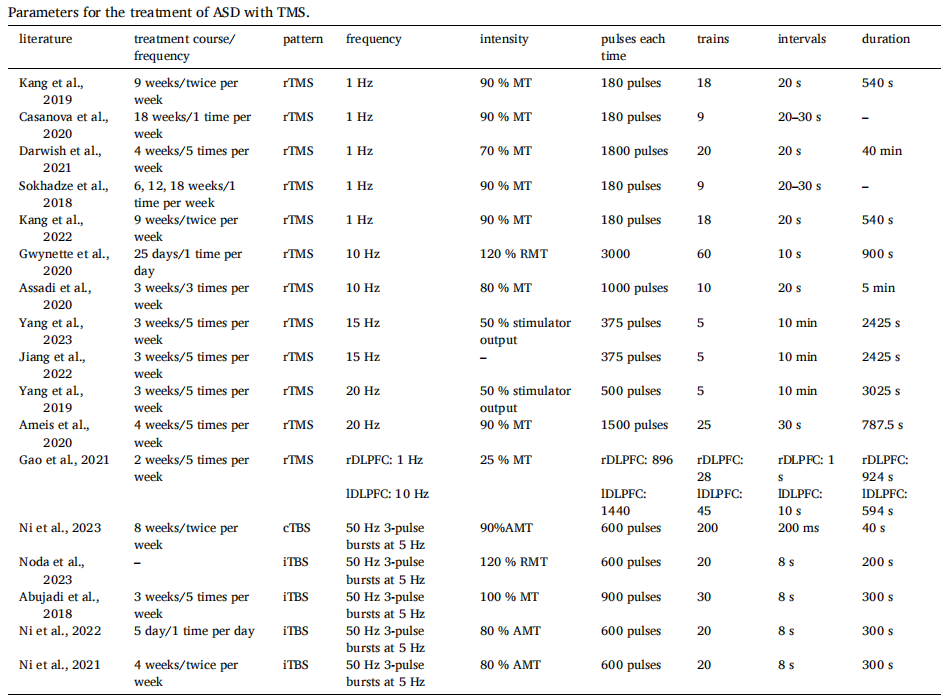
Treatment Session: Among the 17 studies reviewed, 7 reported conducting TMS five sessions per week, making it the most commonly used session number. Other studies adopted different schedules, such as three sessions per week (1 study), twice per week (4 studies), and once per week (2 studies). The total duration varied significantly, ranging from 1 to 18 weeks.
Stimulation Mode: Of the 17 studies, 12 utilized the repetitive TMS (rTMS), which was the most frequently used. Among these, 5 studies employed low-frequency rTMS at 1 Hz. In contrast, the most common high-frequency stimulation frequencies were 10 Hz, 15 Hz, and 20 Hz.
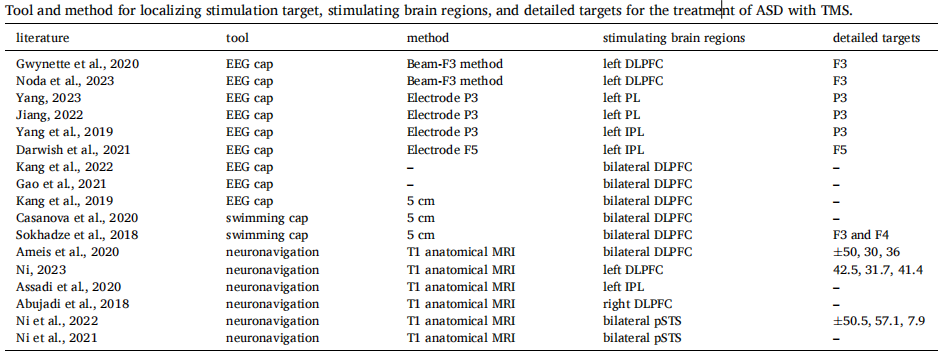
Stimulation Targets and Localization Methods:
The tools used for targeting include EEG caps, swim caps, and neuronavigation based on T1-weighted anatomical MRI. More than half of the studies utilized EEG caps, representing the primary method used so far.
The dorsolateral prefrontal cortex (DLPFC) was the most commonly targeted region. Among the ten studies targeting the DLPFC, six stimulated both hemispheres. Three studies employed the same sequence: stimulating the left DLPFC during the first six sessions, then the right DLPFC, and finally returning to the left DLPFC for the last six sessions.
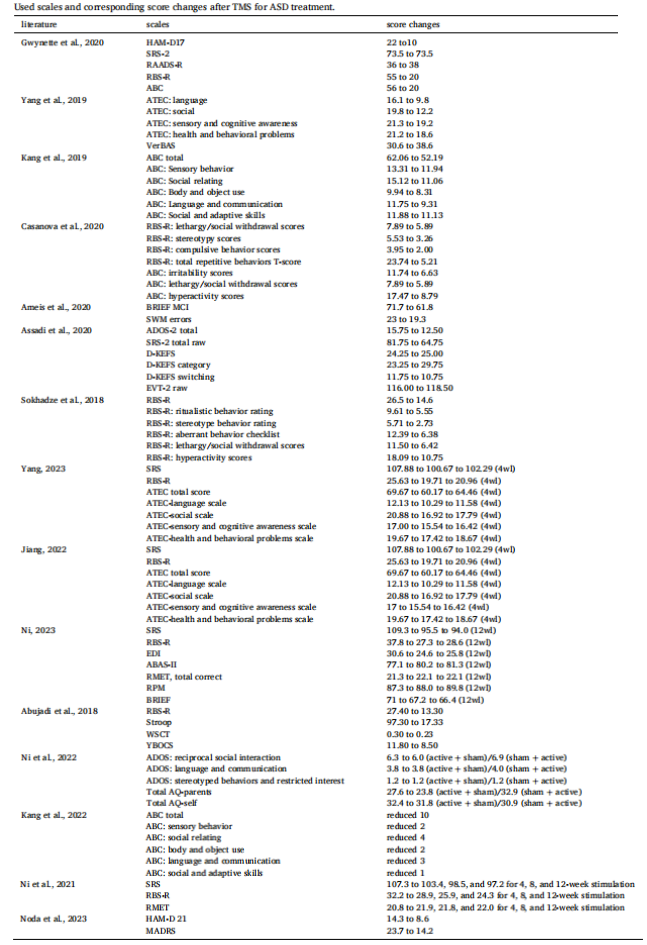
The Repetitive Behavior Scale-Revised (RBS-R) was the primary tool for quantifying changes in behavior. Score reductions ranged from a maximum of 35 points to a minimum of 7.9 points. Among the eight studies, Ni et al. targeted bilateral posterior superior temporal sulcus (pSTS), while the remaining four studies targeted the dorsolateral prefrontal cortex (DLPFC).
Three studies reported changes in stereotyped behaviors after TMS treatment:
Ten studies explored the impact of TMS on language and social behavior scores, using tools such as the Autism Treatment Evaluation Checklist (ATEC), the Social Responsiveness Scale, Second Edition-Adult (SRS-2), and the Aberrant Behavior Checklist (ABC). Among these, six studies reported significant improvements in language and social behaviors.
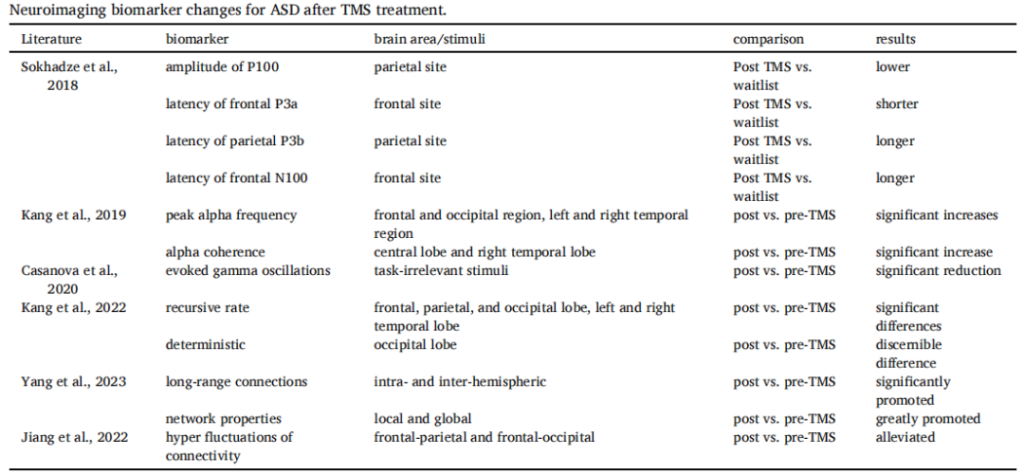
In addition to behavioral assessments, nearly half of the studies reported neurophysiological or task-related outcomes. Key findings include:
These findings highlight the potential of TMS to influence neuroimaging biomarkers, offering valuable insights into its impact on brain connectivity and functional changes in ASD patients.
In summary, since 2018, studies on the use of TMS to treat ASD have demonstrated significant variability in bias risk, stimulation sites, and stimulation parameters. Recent findings generally indicate positive effects of TMS on stereotyped behaviors, repetitive behaviors, language, and social interactions, leading to overall improvements in all assessment scale scores following intervention.
To strengthen the evidence base, future research should prioritize randomized, double-blind, sham-controlled trials. Additionally, to comprehensively evaluate the efficacy of TMS treatment, it is essential to combine routine behavioral assessments with physiological biomarker analysis.

1,This content is organized by the Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd. Criticisms and corrections are welcome. For reprint, please indicate the source.
2.Reference:
Yuan LX, Wang XK, Yang C, Zhang QR, Ma SZ, Zang YF, Dong WQ. A systematic review of transcranial magnetic stimulation treatment for autism spectrum disorder. Heliyon. 2024 May 31;10(11):e32251. doi: 10.1016/j.heliyon.2024.e32251. PMID: 38933955; PMCID: PMC11200348.