Release time :2022-12-15
Source:support@yingchitech.com
Scan:1656
Obsessive compulsive disorder (OCD) is a mental health disorder that affects people of all ages and walks of life, and occurs when a person gets caught in a cycle of obsessions and compulsions[1].
Obsessions are thoughts, images, or impulses that occur over and over again and feel outside of the person’s control.
Compulsions are repetitive behaviors or thoughts that a person uses with the intention of neutralizing, counteracting, or making their obsessions go away.
Most people have obsessive thoughts and/or compulsive behaviors at some point in their lives, but that does not mean that we all have “some OCD.” In order for a diagnosis of OCD to be made, this cycle of obsessions and compulsions must be so extreme that it consumes a lot of time (more than an hour every day), causes intense distress, or gets in the way of important activities that the person values[1].
Research suggests that OCD involves problems in communication between the front part of the brain and deeper structures of the brain. These brain structures use a neurotransmitter (basically, a chemical messenger) called serotonin. Pictures of the brain at work also show that, in some people, the brain circuits involved in OCD become more normal with either medications that affect serotonin levels (serotonin reuptake inhibitors, or SRIs) or cognitive behavior therapy (CBT)[2].
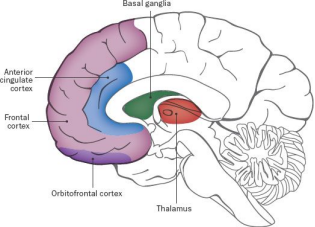
credit: Buckyball Design, Melissa Thomas Baum. Available at https://iocdf.org/about-ocd/what-causes-ocd/
①Cognitive behavioural therapy (CBT) focuses on how your thoughts, beliefs and attitudes affect your feelings and behaviour. You will talk to a therapist, who will help you examine and understand your thoughts and emotions. Over several sessions, CBT can help you stop negative habits, perhaps replacing them with healthier ways to cope.
②Exposure and response prevention (ERP) is specifically designed for OCD. It encourages you to confront your obsessions and resist the urge to carry out compulsions. With this therapy, you do the thing that causes anxiety. The healthcare provider then prevents you from responding with a compulsion.
③Drugs called serotonin reuptake inhibitors (SRIs), selective SRIs (SSRIs) and tricyclic antidepressants may help. They increase levels of serotonin. But it’s inevitable that the drugs may bring some side effects.
For those who don’t benefit from these treatments, or who only experience a minor reduction in symptoms, alternatives have been limited. Over the past decade, transcranial magnetic stimulation (TMS) has emerged as a new option for OCD treatment, and has progressed from a purely experimental treatment to a more widely available therapy backed by research studies demonstrating its effectiveness.
④Transcranial magnetic stimulation(TMS) uses a magnetic device placed on the head. It delivers electrical impulses to the brain. The impulses cause the brain to release chemicals known to improve mood.
TMS is a non-invasive way of “stimulating” (or changing) activity in the brain using magnetic fields. During treatment, patients sit in a chair while a TMS device is pressed against the outside of their head. Inside the device is a wire coil. When an electric current is passed through this coil, it generates a magnetic field. The magnetic field passes through the hair, scalp, muscle, and skull and into the brain, where the magnetic field changes brain activity. This magnetic field can be targeted to reach and stimulate specific areas of the brain, including those involved in OCD. The patient may feel a tapping sensation on their head during treatment, but people receiving TMS are not being “shocked” by electricity. Patients are not sedated during the procedure, discomfort is typically mild, and patients can return to their normal activities immediately.

Double cone coil for psychiatric and neurological disorders associated with dysfunctions of deep brain regions which has gotten positive feedbacks from the doctors: deeper stimulation, benefit earlier, hurts less, making less noise and contact better.

Evidence for rTMS use in obsessive–compulsive disorder (OCD) is accumulating and informing further developments in the neurostimulation field, the latest being deep transcranial magnetic stimulation (dTMS).
2018-FDA approved marketing of deep TMS for OCD[3].
FDA has cleared certain combinations of devices, protocols, and target areas of the brain to be used in treating OCD. The FDA cleared “recipe” for OCD treatment using TMS is as follow:
| Coil | Treatmentarea | Frequency | Intensity | Inter-train Interval | TrainsNumber | Interval | TotalPulses | Total Duration |
| Double-cone | DorsomedialPrefrontal Cortex | 20Hz | 100%MT | 20s | 50 | 20s | 2000 | 18min |
[1] American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association.
[2] International OCD Foundation. What Causes OCD? Available at https://iocdf.org/about-ocd/what-causes-ocd/
[3] FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder. Available at FDA official website: https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder