Release time :2023-07-31
Source:support@yingchitech.com
Scan:1284
Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd.
One of the most challenging clinical problems in the acute treatment of mood disorders: delayed response to treatment. First-line treatments such as medication and psychotherapy usually take several weeks to significantly improve symptoms. Numerous studies have shown that neuromodulatory strategies that act directly on neural circuits may affect depressive symptoms more directly and faster.
Transcranial Magnetic Stimulation (TMS) is a physical neuromodulation method that has been approved by the US Food and Drug Administration (FDA) for more than ten years and is routinely used in clinical practice. However, the current TMS therapy requires daily treatment and takes a long time to respond. Therefore, accelerated transcranial magnetic stimulation has become a new solution to speed up the treatment response.
Accelerated TMS is defined as multiple daily TMS sessions, is an emerging application of TMS aimed at reducing treatment time and improving responsiveness. There is some evidence in the literature that accelerated TMS is comparable in efficacy and safety to FDA-approved TMS for depressive disorders, but research on accelerated TMS is still in its early stages . Currently applied treatment regimens have not been standardized and there are significant differences in core elements.

Preliminary evidence suggests that Accelerated TMS lead to faster improvement in depressive symptoms. This review will discuss nine key elements of accelerated treatment response.
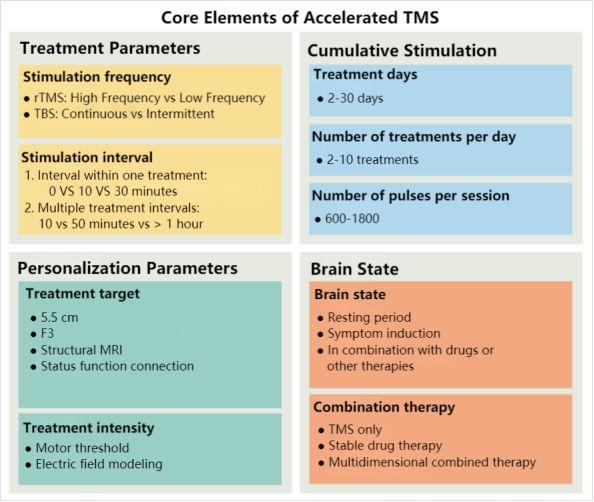
To increase the number of treatments per day, we need to shorten the time required for the current treatment (20-40 minutes) on the premise of ensuring efficacy and safety. As early as 2005, researchers have compared and evaluated the efficacy and safety of theta burst stimulation (TBS) mode and conventional repetitive transcranial magnetic stimulation mode, and found that this TBS mode that simulates the neural activity of endogenous hippocampus can reduce the stimulation time course to one tenth of the original. In 2018, Blumberger et al conducted a non-inferiority randomized clinical trial comparing 3000 pulses of TMS per day with 600 pulses of iTBS, which clearly demonstrated that once-daily iTBS was not inferior to standard TMS, but had the important advantage of reducing treatment time from 37.5 minutes to 3 minutes. The development of TBS protocols has enabled investigators to perform multiple TBS sessions by increasing the number of sessions per day, which is the main reason for accelerating the rapid development of TMS protocols in research and clinical practice.
A conventional TMS regimen is usually one treatment per day with at least 24 hours between treatments. Reducing the stimulation interval can help to speed up the protocol and may enhance the efficacy of certain types of stimulation, such as TBS. By administering three consecutive iTBS treatments of 600 pulses each with a 50-minute interval between each treatment (derived from animal results), Cole and colleagues showed that an hour-long interval between treatments may be the optimal time for TBS to produce long-term potentiation. However, other studies have used treatment intervals as short as 10 minutes and as long as 10 hours, and optimal parameters have not yet been identified. A study investigating the optimal interval showed that 1800 pulses without intervals resulted in a decrease in cortical excitability, whereas 10- and 30-min burst intervals enhanced cortical excitability, with the greatest cortical excitability observed in the 30-min interval group.
An early approach to accelerating TMS was to increase the number of sessions from one session to two sessions. However, in a recent larger randomized controlled trial comparing twice-daily (two 600 pulses) versus once-daily (1200 pulses) iTBS treatments, no significant difference was observed in terms of clinical improvement, and response and remission rates were similar in both groups, suggesting that increasing the number of daily sessions alone (alone) is unlikely to improve treatment outcomes. A recent review by Caulfield et al. summarizes the available data on the use of accelerated TMS regimens. The authors reviewed 63 accelerated TMS studies using 2-10 treatments per day over 2-30 days, with a total number of treatments ranging from 9 to 104. The review provided preliminary evidence that number of treatments per day, total number of treatments and total number of pulses appeared to be positively and linearly related to response rates. However, it is important to note that these parameters are interrelated, as doing more treatments per day means that the total number of treatments and the total number of pulses also increase. Therefore, it is important to understand the interplay between treatment parameters and cumulative stimuli.
The study with the highest number of treatments per day to date was performed by Cole et al. The effect of increasing the number of weekly treatments was investigated by performing ten consecutive TBS stimulations per day. In patients with major depressive disorder (n = 29), Stanford Neuromodulation Therapy (SNT Protocol) was recently FDA-approved following high response rate results, with n = 11 (78.6%) meeting MDD remission criteria and no serious adverse events during the course of treatment for participants. Another study used a similar protocol and found a significant improvement in symptoms of postpartum depression.
Conventional TMS protocols typically stimulate 3000 pulses per day (or 1800 pulses at 1 Hz), but published accelerated TMS studies have employed higher numbers of pulses per day or per treatment. In an open-label trial, Hadley et al. provided a two-week regimen of accelerated 10 Hz high-frequency MDD with 6800 pulses once daily and showed that 33% of patients achieved clinical remission criteria at the end of the study and, importantly, higher doses of TMS were well tolerated without significant adverse outcomes. Cole et al. provided the protocol with the highest number of pulses per treatment, stimulating 9000 pulses per treatment, ten times per day, for a total of 90000 pulses per day, which demonstrated that a high number of pulses can guarantee safety when the treatment interval is 50 minutes.
With magnetic resonance imaging (MRI), targets for TMS therapy can be individualized. Functional connectivity (FC) networks connect neural regions with projections on the cortex, and TMS is applied to regions of the skull corresponding to the cortex to "target" stimulation of neural structures. FC analysis is typically performed using resting-state (RS) fMRI scans to define individual TMS therapeutic targets. In an accelerated TMS protocol, FC was used in patients with a negative correlation pattern in the subgenital anterior cingulate cortex (sgACC) at baseline, which was reversed after accelerated TMS treatment, but not in non-responding patients. According to the theory that cortical regions are connected to deeper brain regions through functional networks, the region within the LDLPFC that has the strongest negative correlation with sgACC is the optimal target.
Combining resting-state FC-based localization with electric field (E-field) modeling may be another approach to optimize TMS target location and coil orientation. Electric field modeling uses individual structural image scans to control the position and orientation of the coil to approximate the direction and magnitude of the induced currents in the brain. This method reduces inter-individual variability between stimulus location and ideal coil orientation, and reduces the distance between the stimulus target and the ideal acting cortex. Results of validation studies of this approach suggest that individualized targeting may maximize clinical efficacy and help predict treatment response. Other ongoing studies aim to optimize stimulation parameters according to the cortical electric field of different individuals. However, this method also has shortcomings, and some individuals may require an intensity exceeding the standard 120% motor threshold, and the safety of TMS therapy (including iTBS) exceeding the threshold intensity is an important factor.
Is there an interaction between brain state (i.e., an individual's state of mind or emotion) and the effects of brain stimulation? Studies have shown that the effects of TMS may vary depending on the brain environment. For example, in the treatment of obsessive-compulsive disorder, it is a common method to induce symptoms before TMS treatment. Altering the state of the brain can also be done by combining TMS with drugs. Other options include combining TMS with various psychotherapies. Although whether and how these approaches are combined remains an unanswered question, some evidence suggests that the type and timing of psychotherapy may be important.
Whether, and how, drugs have an effect on the clinical outcomes of accelerated TMS is unclear. In earlier randomized controlled trials of TMS alone, participants had improved clinical outcomes when they used antidepressants after the trial, suggesting a synergistic effect between the two. There are currently no data from studies suggesting that the efficacy of TMS for MDD is reduced when patients are taking antiepileptic drugs, benzodiazepines, or antipsychotics, and may be improved when patients are taking psychostimulants.
1.Interpretation of literature | Beyond the efficacy of transcranial magnetic stimulation in peripartum depression: A systematic review exploring perinatal safety for newborns
2.The progress of a serial researches on "rTMS treatment of insomnia disorder" assisted by YINGCHI