Release time :2024-07-22
Source:support@yingchitech.com
Scan:622
Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd.
01 Application of TMS in children and adolescents with psychiatric disorders
02 Application of TMS in children with cerebral palsy
03 Application of TMS in autism spectrum disorder
04 Application of TMS in autism with comorbid refractory depression
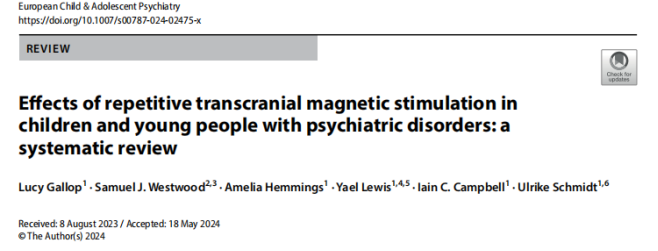
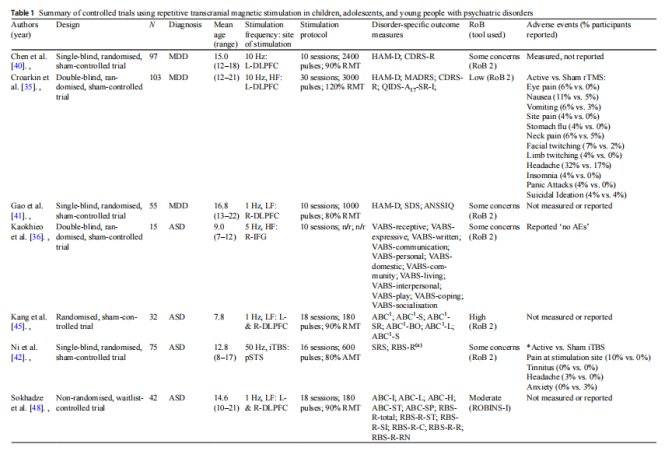
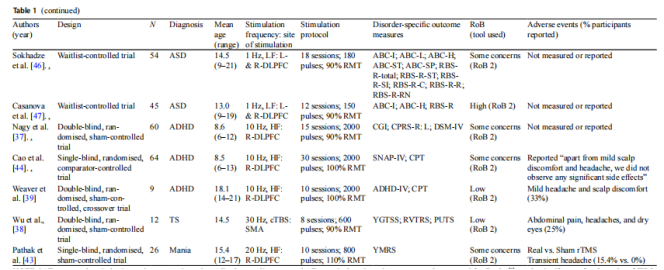
This review systematically reviewed studies on the effects of repetitive transcranial magnetic stimulation (rTMS) on child and adolescent psychiatric disorders (78 studies, 1389 participants, aged 3-25 years, covering major depressive disorder, autism spectrum disorder, schizophrenia, obsessive-compulsive disorder, tourette syndrome, attention deficit hyperactivity disorder, borderline personality disorder, anorexia, binge eating disorder, catatonia, and internet gaming addiction) to
(1)assess the effects of rTMS on disorder-specific symptoms and impairments,
(2)determine the effects of rTMS on mood and neurocognitive outcomes,
(3)summarize the populations and methods studied in ongoing trials and unpublished data.
Study on the application of TMS in children and adolescents
Repetitive transcranial magnetic stimulation (rTMS) is a new potential treatment tool for cerebral palsy (CP) with the ability to reduce spasticity and improve patients' gait patterns.
(1)A study on children with spastic cerebral palsy used a stimulation protocol of high-frequency rTMS (5Hz or 10Hz), 15 minutes per treatment, 1500 pulses in total, and 20 days in a course of treatment. It was observed that muscle spasticity was significantly reduced and hand function was significantly enhanced. The lower frequency (5Hz) was more effective for hemiplegic CP patients in the 2-6 age group, while the higher frequency (10Hz) had a restorative effect on hemiplegic and quadriplegic patients in the older age group.
(2)A child with CP with mild ataxia was treated on the right dorsolateral prefrontal cortex for 8 months, 5 days a week, at a frequency of 0.5 Hz (a single treatment included 5 sets of pulses, each set of 121 pulses), after rTMS treatment , motor and cognitive functions as well as functional network connections were gradually improved.
(3)1Hz rTMS was administered to the contralateral primary motor cortex of patients with hemiplegic CP for 3 weeks, 4 days per week - the results showed that low-frequency rTMS could induce changes in white matter structural connectivity and improve the patients' motor function. Increasing the number of treatments at a constant frequency over a period of time can also significantly improve the recovery of motor function.
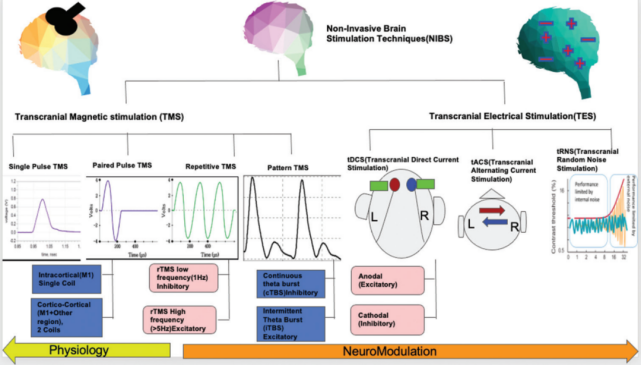
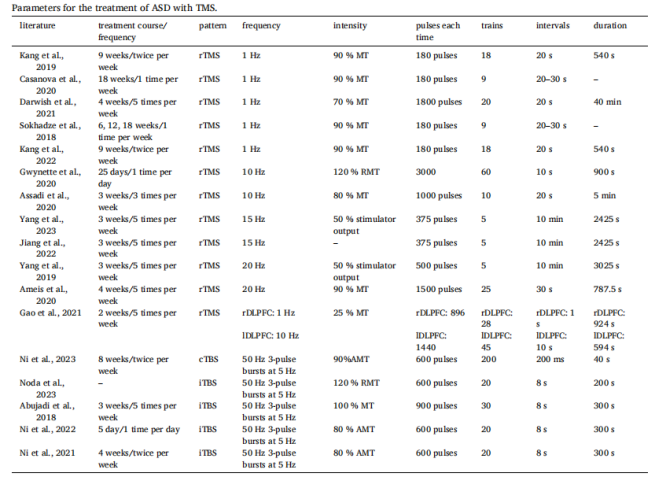
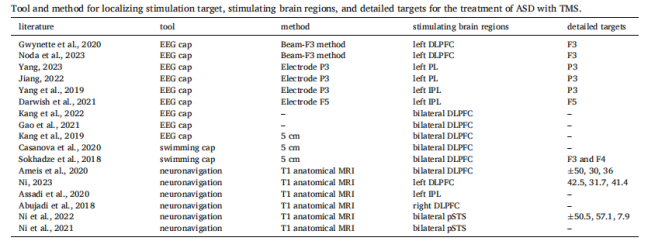
This review included 17 articles published after 2018, including 7 randomized controlled trials and 10 open-label studies. Overall, studies on TMS for the treatment of autism spectrum disorder (ASD) showed significant diversity in terms of bias risk, stimulation target, stimulation parameters, etc. However, the results generally showed that TMS had a positive effect on stereotyped behaviors, repetitive behaviors, speech, and social aspects of ASD, and all scale scores were improved overall after intervention. To strengthen the evidence base, future studies should give priority to randomized, double-blind, sham-controlled trials. In addition, in order to more comprehensively evaluate the efficacy of TMS, changes in physiological indicators must be included in addition to routine behavioral assessments.
TMS protocol parameters for ASD
Stimulation targets and positioning methods for TMS treatment of ASD
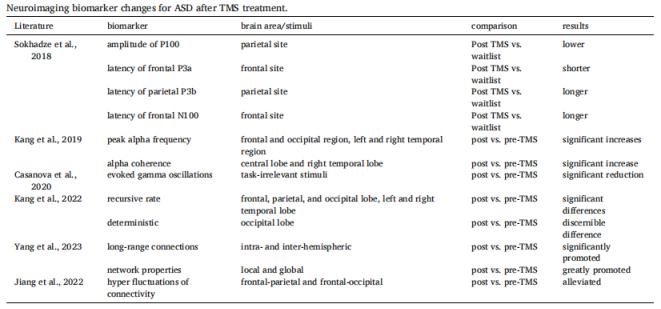
Changes in neuroimaging markers after TMS treatment for ASD
IF=4.0 | Assessing the impact of repetitive transcranial magnetic stimulation on effective connectivity in autism spectrum disorder: An initial exploration using TMS-EEG analysis
This study used transcranial magnetic stimulation combined with electroencephalography to explore the rTMS-induced changes in effective connectivity in children with autism spectrum disorder (ASD) - TMS-EEG data before and after rTMS treatment were obtained from 12 children diagnosed with ASD. The intervention protocol was: high-frequency 15Hz rTMS to the left parietal lobe, stimulation time 5s, interval time 10min, a total of 375 pulses, 5 days a week, for 3 weeks, a total of 15 treatments. Dynamic EEG network analysis showed that after rTMS intervention, long-range feedback connections in the brain of ASD patients (such as frontal lobe to parietal lobe area, frontal lobe to occipital lobe area, frontal lobe to posterior temporal lobe area) were strengthened, while short-range connections (such as bilateral occipital lobe area, occipital lobe to posterior temporal lobe area) were weakened. The changes in clinical scale scores after treatment were consistent with the changes in brain network connectivity, and basic ASD symptoms were also improved accordingly.
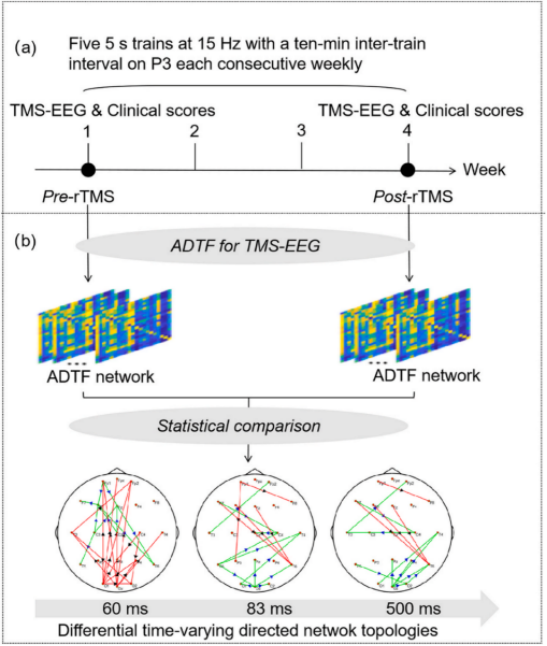
Study design: (a) rTMS intervention. (b) Effective connectivity analysis
Treatment of refractory depression in ASD is very challenging and often requires multiple medications or treatments with high side effects. Although the efficacy of rTMS for refractory depression has been well established, large-scale interventions in ASD remain challenging. This open-label trial demonstrated the efficacy and safety of accelerated Theta Burst Stimulation (aTBS) for the treatment of refractory depression in patients with ASD.
Intervention
Protocol:
① Bilateral stimulation group: iTBS of the left dorsolateral prefrontal cortex + cTBS of the right dorsolateral prefrontal cortex, 600 pulses each, 90% RMT ( measured in both hemispheres separately) , 3 times a day.
②Unilateral stimulation group: iTBS of the left dorsolateral prefrontal cortex, 600 pulses, 90% RMT, 3 times a day.
Considering the subjects with sensory hypersensitivity, during the first two days of treatment, the intensity of stimulation was started from 50% RMT and gradually increased by 10-20% each time to the target stimulation intensity (90% RMT) according to the tolerance of each subject.
Primary outcome: HDRS-17 scale.
Secondary outcomes: Beck Depression Inventory-II (BDI-II); Quick Inventory of Depressive Symptomatology (QIDS); physician-administered Columbia-Suicide Severity Rating Scale (C-SSRS); Suicide Behavior Questionnaire (SBQ); Generalized Anxiety Disorder-7 item (GAD-7); Pittsburgh Sleep Quality Inventory (PSQI); Social Responsiveness Scale (SRS); NIH Cognitive Toolbox.
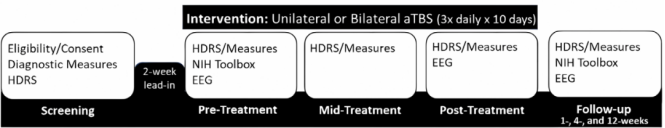
The primary outcome showed that aTBS treatment was associated with significant, substantial, and sustained improvements in depressive symptoms regardless of stimulation site. Other secondary outcomes, including self-report depression scales, fluid cognition and sleep quality, also showed significant improvements.

aTBS was effective and well tolerated in patients with ASD and comorbid MDD. However, a larger, randomized, sham-controlled trial is needed to further evaluate the efficacy of aTBS in this population.

This content is organized by the Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd. Criticisms and corrections are welcome. For reprint, please indicate the source.