Release time :2022-10-26
Source:support@yingchitech.com
Scan:1979

Obsessive-Compulsive Disorder is characterised by the presence of persistent obsessions or compulsions, or most commonly both. Obsessions are repetitive and persistent thoughts, images, or impulses/urges that are intrusive, unwanted, and are commonly associated with anxiety. The individual attempts to ignore or suppress obsessions or to neutralize them by performing compulsions. Compulsions are repetitive behaviours including repetitive mental acts that the individual feels driven to perform in response to an obsession, according to rigid rules, or to achieve a sense of ‘completeness’. In order for obsessive-compulsive disorder to be diagnosed, obsessions and compulsions must be time consuming (e.g. taking more than an hour per day) or result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.[1]
OCD has an estimated lifetime prevalence of 2–3% under DSM-III, DSM-III-R and DSM-5 criteria. Some epidemiological surveys of US and European citizens, using diagnostic instruments aligned with the DSM-IV, produced more conservative estimates of lifetime prevalence of respectively 1.6% and 0.8%. Another epidemiological survey, possibly capturing a broader spectrum of cases, estimated the lifetime prevalence at 5.8% and 6.2% in low and high income countries respectively. Indeed, other epidemiological surveys have estimated the prevalence of subclinical OC syndromes at between 7–25%. Fullana et al. (2009) analysed the 20-year prospective Dunedin study of an unselected birth-cohort aged 11–32 years. Consistent with the US National Comorbidity data, DSM-IV OCD was reported in 2.3% of the sample at age 26 years and 1.8% at age 32 years, whereas sub-syndromal obsessions and compulsions, affecting up to 25% of the cohort, were also found to be associated with significant impairment and help-seeking behaviour.[2]


TMS is a non-invasive neuromodulation technology. The time-varying pulsed magnetic field can penetrate the skull non-invasively, act on the central nervous system, generate induced currents, and cause a series of physiological and biochemical reactions, thereby affecting metabolism and neuronal excitability in the brain so that improve and treat mental and neurological diseases.
In general, high-frequency stimulation increases the cortical excitability, whereas low-frequency stimulation has inhibitory control on the neural circuits. High-frequency rTMS (>5 Hz) produces an excitatory effect on neural tissue by inducing a form of long-term potentiation (LTP) that increases efficacy at the synapse that can last beyond the duration of a treatment session. Lowfrequency rTMS (≤1 Hz) produces an inhibitory effect on neural tissue via a long-term depression(LTD)-like mechanism.
This clinical study proves that TMS is a promising tool for treatment of OCD.
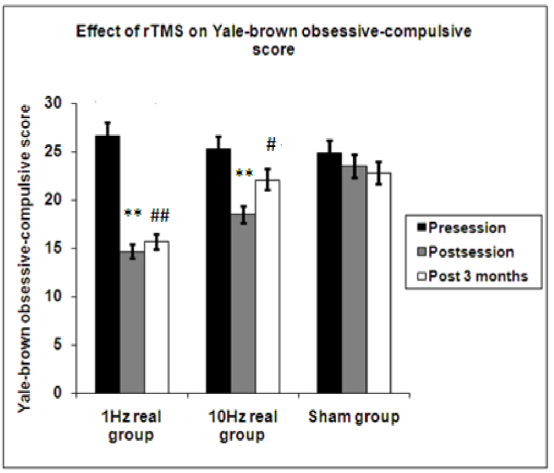
The primary measuring system used in this study was the Yale-Brown Obsessive-Compulsive Scale (YBOCS). In group 1 patients who received (1 Hz) rTMS sessions there was highly significant decrease in the score of YBOCS after session and this improvement was maintained for 3 months. There was significant improvement in the score in group 2 who received 10 Hz after the end of session(P=0.004). This improvement was not maintained for 3 months (P=0.174), while no changes were recorded among sham group neither after the end of session nor after 3 months.[3]
TMS can effectively treat obsessive-compulsive disorder for up to 3 months.
| Disease | Stimulation mode | Stimulation site | Stimulation frequency (Hz) | Stimulation intensity | Stimulation time (s) | Interval time (s) | Total number of pulses |
| OCD | LF-rTMS | R-DLPFC | 1 | 100%RMT | 500 | 40 | 2000 |

[4]
[1] WHO. International Classification of Diseases 11th Revision. 2022.
[2] Fineberg, N. A., Dell'Osso, B., Albert, U., Maina, G., Geller, D., Carmi, L., ... & Zohar, J. (2019). Early intervention for obsessive compulsive disorder: an expert consensus statement. European Neuropsychopharmacology, 29(4), 549-565.
[3] Elbeh, K., Elserogy, Y., Khalifa, H. E., Ahmed, M. A., Hafez, M. H., & Khedr, E. M. (2016). Repetitive transcranial magnetic stimulation in the treatment of obsessive-compulsive disorders: Double blind randomized clinical trial. Psychiatry research, 238, 264–269. https://doi.org/10.1016/j.psychres.2016.02.031
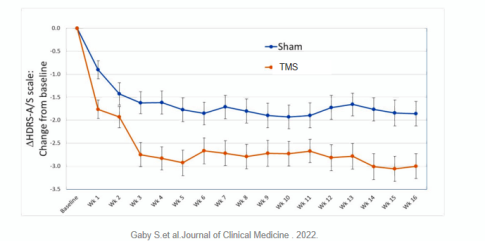
[4] Pell, G. S., Harmelech, T., Zibman, S., Roth, Y., Tendler, A., & Zangen, A. (2022). Efficacy of deep TMS with the H1 coil for anxious depression. Journal of clinical medicine, 11(4), 1015.